Irritable Bowel Syndrome (IBS). Exploring the Intricate Relationship Between the Brain and Gut
- Valentina

- Feb 25, 2024
- 5 min read
Updated: Feb 26, 2024
Introduction:
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder that affects millions of people worldwide, around 1 in 10 people in the UK. Despite its prevalence, IBS can be challenging to understand and very hard to manage due to its varied symptoms and complex underlying factors. The age-old saying, "Trust your gut," holds more truth than we might realize. Beyond its literal meaning, our gut has a profound impact on our mental and emotional well-being, thanks to the intricate communication network known as the brain-gut axis. In this blog, we'll explore the fascinating interplay between emotions and gut health and how therapy can help.
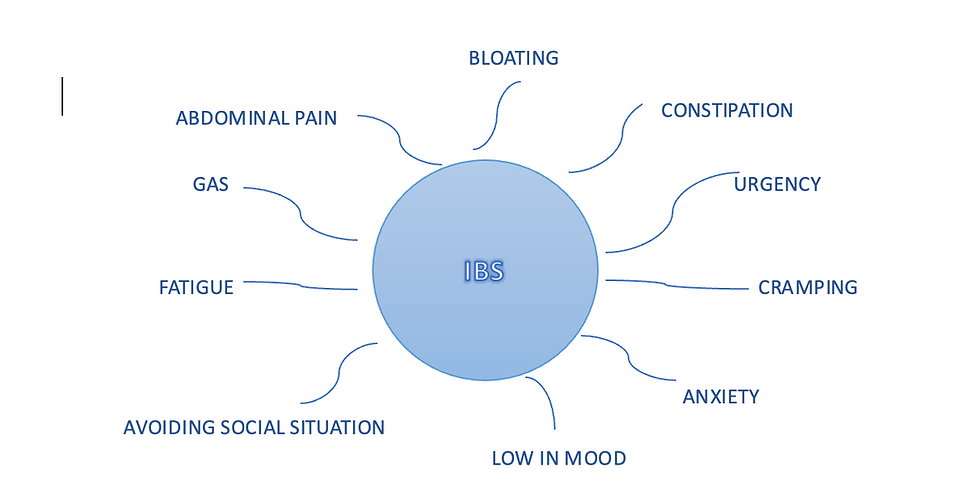
Main Symptoms of IBS:
IBS manifests differently from person to person, but some common symptoms include:
Abdominal pain or cramps, often relieved by bowel movements
Abdominal fullness or bloating
Changes in bowel habits, such as disordered defecation (e.g. diarrhoea, constipation, or both)
Urgency to use the bathroom
While the exact cause of IBS remains unknown, it's believed to involve a combination of genetic, environmental, and psychological factors.
The Impact of Emotions on Gut Health:
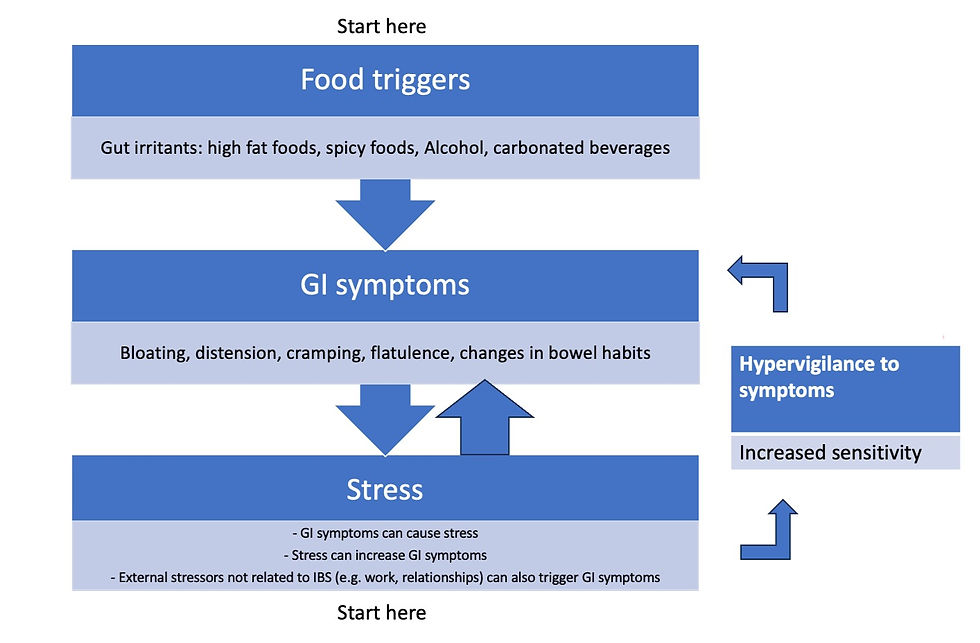
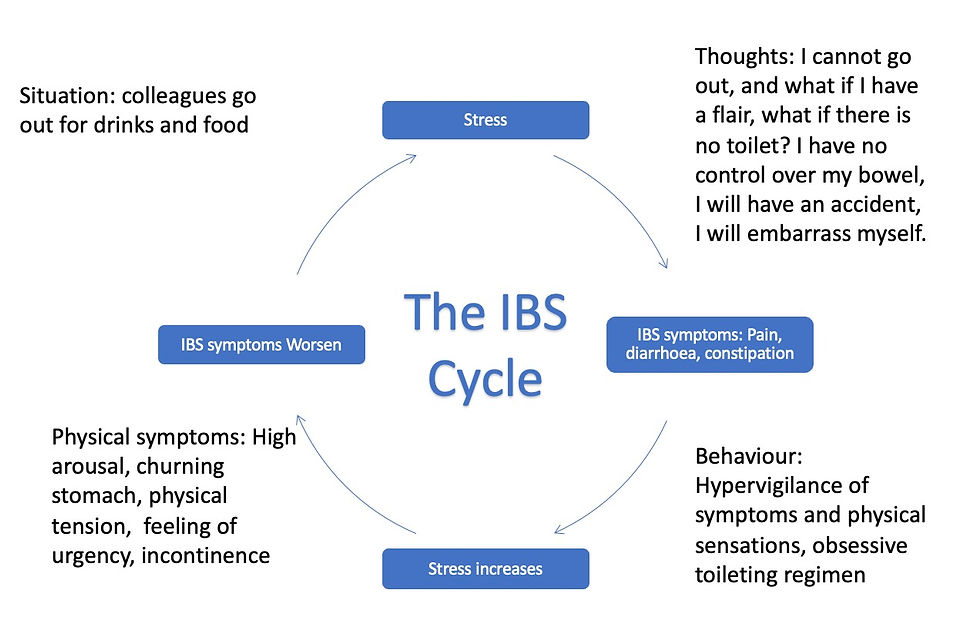
The relationship between emotions and gut health is a complex and bidirectional one. Stress, anxiety, and other emotional factors can significantly impact gut function and exacerbate symptoms of IBS. When we experience stress or negative emotions, our brain releases signaling molecules that can affect the gut's motility, secretion, and sensitivity. This can lead to symptoms such as abdominal pain, bloating, and altered bowel habits.
Conversely, disturbances in gut microbiota or gastrointestinal discomfort can send signals to the brain, influencing mood and cognitive function. This bidirectional communication, known as the brain-gut axis, highlights the interconnectedness of our mental and digestive health.
Navigating the Brain-Gut Connection:
Understanding the brain-gut connection is crucial for effectively managing IBS and improving overall well-being. By recognizing the impact of emotions on gut health and vice versa, individuals with IBS can take proactive steps to reduce stress, manage symptoms, and enhance their quality of life.
Our nervous system operates in two distinct modes. In a state of calmness, various physiological changes occur, including a decrease in heart rate, increased salivation, slower breathing, constricted pupils, stimulated digestion, and normal bowel function. This state is commonly referred to as "rest and digest."
Conversely, when we experience stress or agitation, our heart rate rises, the mouth becomes dry, breathing accelerates, pupils dilate, and digestion slows. In this scenario, the large intestine may attempt to empty rapidly, leading to a sense of urgency. This indicates that the nervous system is in a fight or flight mode, which is beneficial for situations like pursuing prey, defending against attackers, or escaping danger.....but not so great for for digestion or IBS.
Stress can significantly impact the digestive system by delaying the movement of food through the stomach and upper small intestine while stimulating how quickly food is pushed through our lower bowels. Essentially, heightened anxiety leads to a slowdown in digestion, potentially resulting in the need for a bowel movement.
Strategies for managing IBS and nurturing the brain-gut connection may include:
Adopting stress-reduction techniques such as mindfulness meditation, deep breathing exercises, or yoga
Following a balanced diet that includes fiber-rich foods, probiotics, and adequate hydration
Engaging in regular physical activity to promote digestion and alleviate stress
Seeking support from healthcare professionals, including gastroenterologists, dietitians, and psychologists.
Common psychological responses that can exacerbate symptoms
In Irritable Bowel Syndrome (IBS), hypervigilance and avoidance are common psychological responses that can exacerbate symptoms and impact overall well-being.
Hypervigilance: Hypervigilance refers to a heightened state of awareness or vigilance regarding bodily sensations and symptoms. Individuals with IBS may become hyper-focused on their digestive system, constantly monitoring for any signs of discomfort, pain, or changes in bowel habits. Hypervigilance can contribute to a cycle of heightened anxiety and physiological arousal, potentially exacerbating IBS symptoms.
Avoidance: Avoidance involves actively steering clear of situations, activities, or foods that are perceived as potential triggers for IBS symptoms. This avoidance behaviour may stem from a desire to prevent discomfort or embarrassment associated with symptom flare-ups.
While avoidance behaviours may provide temporary relief from symptoms, they can also perpetuate anxiety and reinforce a cycle of fear and avoidance, ultimately limiting individuals' quality of life and engagement in meaningful activities.
The Role of therapy
Cognitive-Behavioral Therapy (CBT): Cognitive-behavioral therapy (CBT) is a proven therapeutic approach that focuses on changing negative thought patterns and behaviors to improve mental health. In the context of brain-gut interaction, CBT can be instrumental in managing conditions like irritable bowel syndrome (IBS), which often have a strong psychological component. By addressing stress, anxiety, and maladaptive coping strategies, CBT helps regulate the brain-gut axis, leading to symptom relief and improved quality of life. CBT techniques, such as cognitive restructuring and relaxation exercises, empower individuals to challenge negative beliefs about their symptoms and develop healthier coping mechanisms. Moreover, CBT interventions tailored to gastrointestinal disorders incorporate education about the brain-gut connection, helping patients understand how emotions impact gut function and vice versa. This knowledge fosters a sense of control and empowerment, reducing anxiety and enhancing resilience in the face of digestive challenges.
Mindfulness Mindfulness techniques, such as mindfulness meditation and body scan exercises, can help individuals with IBS cultivate present-moment awareness without judgment. By practising mindfulness, individuals can learn to observe bodily sensations without reacting with fear or anxiety.
Acceptance and Commitment Therapy (ACT) ACT encourages individuals to acknowledge and validate uncomfortable thoughts, feelings, and sensations related to IBS while pursuing valued life goals and activities. ACT fosters psychological flexibility. By developing flexibility in responding to internal and external experiences, individuals can adaptively cope with the challenges of living with IBS and improve their overall resilience and well- being.
Helpful souce of information:
Conclusion:
Irritable Bowel Syndrome (IBS) is a prevalent gastrointestinal disorder that can significantly impact quality of life. By understanding the main symptoms of IBS and the intricate relationship between emotions and gut health, individuals can take proactive steps to manage their condition effectively. Through a combination of lifestyle modifications, stress reduction techniques, and professional support, those living with IBS can navigate their symptoms and nurture a healthy brain-gut connection for improved well-being. By recognizing this relationship and harnessing the therapeutic benefits of approaches like cognitive-behavioural therapy, we can foster harmony within the brain-gut axis, promoting both physical and emotional well-being. Trusting our gut isn't just about intuition, it's about nurturing a holistic understanding of ourselves and embracing the profound interplay between our thoughts, emotions, and digestive health.




Comments